
Hospital Beds for Diabetes: Tips for Better Homecare
Diabetes is a chronic condition that affects millions of people worldwide, and its impact goes far beyond just managing blood sugar levels. The disease can lead to a variety of complications, some of which are severe and can dramatically affect a person’s quality of life. In this article, we will also discuss how homecare, particularly the use of hospital beds, plays a crucial role in managing the condition. From helping with wound care and mobility issues to improving comfort and sleep, hospital beds offer essential support for diabetic patients at home. We’ll also discuss the importance of frequent repositioning and provide practical tips for managing diabetes more effectively with a hospital bed.
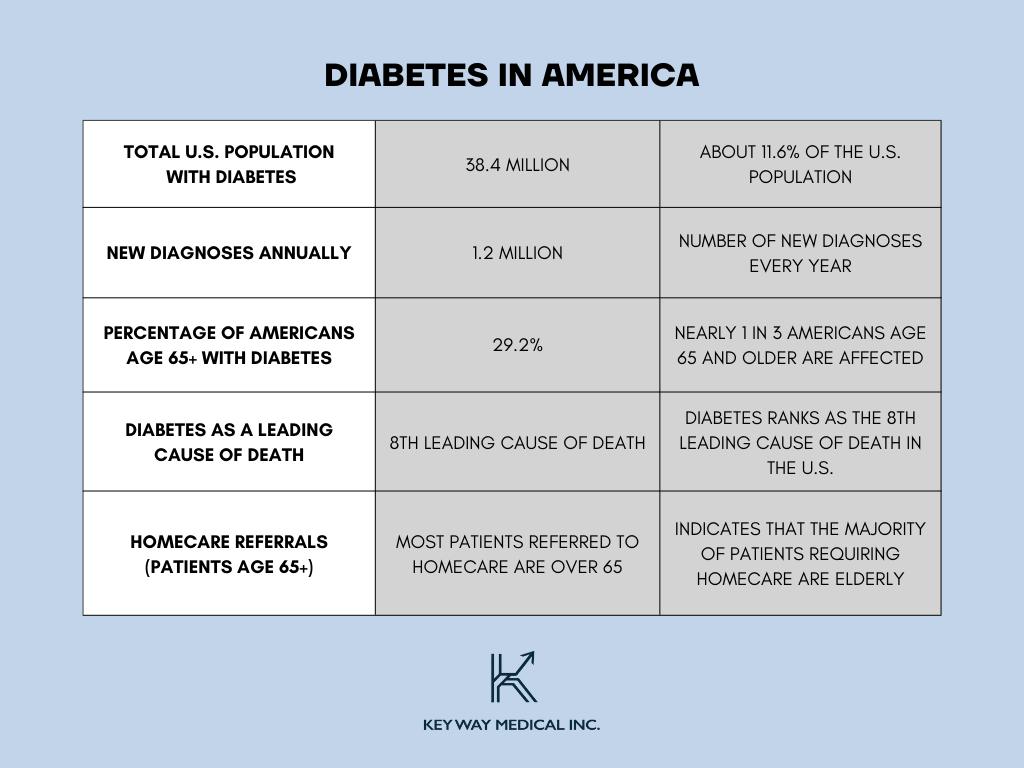
Diabetes in America: An Overview of Prevalence, New Diagnoses, and the Aging Population
Diabetes is becoming more common in the U.S., affecting millions of people. It puts a strain on the healthcare system, leading to higher medical costs. As more people live with diabetes, it also affects productivity, with many needing time off for treatment possibly resulting in needing homecare assistance.
CDC. (2024). National Diabetes Statistics Report. Retrieved from: https://www.cdc.gov/diabetes/php/data-research/index.html
Harvard University. (2024). National Diabetes Statistica Report 2024. Retrieved from: https://repository.gheli.harvard.edu/repository/11854/#:~:text=The%20National%20Diabetes%20Statistics%20Report,with%20diabetes%20increased%20to%2029.2%25.
American Diabetes Association. (2023). Statistics About Diabetes. Retrieved from: https://diabetes.org/about-diabetes/statistics/about-diabetes#:~:text=New%20cases:%201.2%20million%20Americans,18%20and%20older%20had%20prediabetes.
As of 2025, diabetes affects an estimated 38.4 million Americans or about 11.6% of the population. This chronic condition is increasingly prevalent, with 1.2 million new diagnoses occurring each year. The impact is especially significant among older adults, with nearly 30% of Americans aged 65 and older living with diabetes.
Diabetes is also a leading cause of death in the U.S., ranking as the 8th most common cause. With this growing health crisis, more patients—especially those over 65—are being referred to homecare services for support in managing their condition. For these patients, a hospital bed in the home can play a crucial role in improving comfort, promoting safety, and enhancing overall care. With proper homecare, including specialized equipment like hospital beds, managing diabetes at home can help improve quality of life, reduce hospital readmissions, and ensure patients receive the care they need in a familiar, supportive environment.
Little-Known Facts About Diabetes
While most people understand that diabetes is a condition where the body struggles to regulate blood sugar, there are other surprising aspects of the disease to consider:
- Diabetic Eye Disease Can Cause Blindness: Diabetic retinopathy is one of the leading causes of blindness among adults. This condition occurs when high blood sugar levels damage the blood vessels in the retina, leading to vision loss.
- Diabetes Affects More Than Just the Pancreas: Diabetes is often thought of as a disease that only affects blood sugar and insulin production. However, it can lead to a domino effect of complications that impact the kidneys, heart, eyes, and even the nervous system.
How Homecare and Diabetes Management Connect
Managing diabetes effectively requires a well-rounded approach that includes regular monitoring, sticking to prescribed medications, making lifestyle changes, and ongoing education. Homecare plays an essential role in supporting people with diabetes by providing personalized care that addresses the daily challenges of living with the condition.
Homecare services can assist with important tasks like checking blood sugar levels, administering medications, helping with meal planning, and offering guidance on physical activity. These services ensure patients stay on track with their treatment plans.
Caregivers also help identify early signs of complications, such as nerve damage or infections and can take action quickly to prevent further issues. For those with long-term diabetes, homecare offers consistent support that helps avoid unnecessary hospital visits, improves overall quality of life, and encourages independence while keeping health outcomes stable.
The Domino Effect: How Diabetes Leads to Mobility Issues
Diabetes can lead to mobility issues due to complications like neuropathy, joint stiffness, and poor circulation, making it harder for individuals to walk, balance, and manage blood sugar levels. A great solution for this would be a hospital bed with adjustable positions that can provide relief by reducing pressure on affected areas, supporting proper alignment, and improving comfort, which helps diabetic individuals better manage their condition and enhance their overall quality of life.
In this way, a hospital bed not only helps with mobility challenges but also plays a critical role in the broader effort to manage diabetes and its associated complications. Here are some tips to help prevent mobility issues with diabetes:
Encourage Physical Activity
Depending on the patient’s condition, simple exercises like walking, stretching, or gentle strength training can help improve circulation and maintain mobility. Some exercises can even be done while in their bed.
Tailored Exercise Plans: A healthcare professional can create a safe and effective exercise program based on the individual’s specific condition and limitations. This may include gentle stretches, low-impact exercises like walking or swimming, or even chair exercises that can be done from bed.
Start Low, Go Slow: It’s crucial to begin with low-intensity activities and gradually increase duration and intensity to avoid overexertion. Even small increases in daily activity can significantly improve blood sugar control and overall well-being.
Focus on Flexibility: Gentle stretching exercises can help maintain joint mobility and range of motion, making daily activities easier and reducing the risk of falls.
Provide Foot Support
Ensuring that your patient wears properly fitted shoes and insoles can help prevent further damage to the feet and improve their ability to walk.
Properly Fitted Shoes: Regular visits to a podiatrist are essential for diabetic patients. They can assess foot health, prescribe custom orthotics if needed, and recommend properly fitted shoes that provide optimal support, pressure relief, and prevent further foot damage.
Inspect Feet Daily: Look for any signs of redness, blisters, cuts, or swelling on the feet daily. Early detection of foot problems can prevent serious complications like diabetic foot ulcers.
Moisturize: Dry, cracked skin on the feet can increase the risk of infection. Using a fragrance-free moisturizer regularly can help keep the skin healthy.
Install Safety Features at Home
Adding grab bars, ramps, and non-slip rugs can help a diabetic patient move around the home more safely and independently.
Grab Bars: Install grab bars in strategic locations like bathrooms, near showers, and next to stairs to provide additional support and stability when standing or transferring.
Non-Slip Rugs: Use non-slip rugs in bathrooms and kitchens to prevent falls on wet surfaces.
Lighting: Ensure proper lighting throughout the home to improve visibility and reduce the risk of tripping or bumping into obstacles.
Furniture Placement: Arrange furniture to create clear walkways and avoid clutter that could cause tripping hazards.
Monitor for Early Signs of Mobility Decline
Be vigilant for signs of reduced mobility, such as difficulty standing up or walking, and address these concerns early on.
Observe Gait Changes: Pay attention to any changes in gait, such as shuffling, difficulty walking in a straight line, or taking smaller steps.
Increased Difficulty with Daily Tasks: Notice if the individual has trouble with daily tasks like getting dressed, bathing, or climbing stairs.
Pain or Stiffness: If the patient experiences increased pain or stiffness in the joints or muscles, it’s important to report it to the healthcare professional. Early intervention can help prevent further complications.
Regular Checkups: Scheduling regular checkups with a doctor or physical therapist allows for monitoring of mobility and potential interventions to maintain independence.
How Hospital Beds Can Aid in Homecare for Diabetic Patients
Hospital beds designed for home care are essential in managing diabetic conditions, offering both comfort and support to patients at risk for complications like pressure sores, poor circulation, and mobility issues. These specialized beds not only make daily care tasks easier for both patients and caregivers but also provide crucial benefits for managing the unique challenges of diabetes such as:
- Pressure Relief: Adjustable positions help reduce pressure on vulnerable areas (hips, tailbone, heels) to prevent diabetic bed sores.
- Improved Circulation: Elevating or lowering the head and foot of the bed promotes better blood circulation, aiding overall comfort and health.
- Enhanced Mobility: Beds designed for easy repositioning help improve mobility and reduce strain, especially for patients with limited movement.
- Easier Caregiver Assistance: Adjustable settings allow caregivers to assist with routine tasks like repositioning, administering medications, and personal care with less physical strain.
- Better Quality of Life: Hospital beds support diabetic patients in managing their condition effectively, leading to greater independence and a higher quality of life.


Hospital Beds and Diabetic Wound Care: Enhanced Home Treatment
Hospital beds designed for home care play a crucial role in improving wound care by offering features that promote comfort, support, and easier access for treatment. Let’s explore some of the key ways these beds enhance wound healing and make care more efficient for both patients and caregivers!
- Improved Circulation: The ability to elevate or reposition the bed helps improve circulation, which is crucial for diabetic wound healing.
- Easier Wound Care: Adjustable positions make it simpler for caregivers to access and dress wounds, reducing strain on both the patient and caregiver.
- Pressure Ulcer Prevention: Specialized mattresses help prevent new pressure ulcers, protecting the skin and improving healing.
The Importance of Quality Rest: How a Hospital Bed Can Support Diabetic Patients
Proper rest is essential for diabetic patients to manage their condition and promote healing, and hospital beds designed for home care provide the features necessary for a restful and supportive sleep environment. These beds offer adjustable positions and pressure-relieving mattresses, addressing common issues like discomfort from neuropathy, poor circulation, and the risk of pressure ulcers, ultimately providing more restful sleep.
Here’s how hospital beds offer comfort, sleep, and support:
- Adjustable Positions: Allows patients to find a comfortable posture, reducing discomfort from diabetic neuropathy and promoting better rest.
- Improved Circulation: Elevating the legs can reduce swelling and improve blood flow, common concerns for diabetic individuals.
- Pressure-Relieving Mattresses: Help minimize the risk of pressure ulcers by reducing pressure on vulnerable areas, supporting skin integrity and healing.
- Customizable Comfort: Enhances sleep quality, leading to better blood sugar regulation, recovery, and overall well-being.
Supporting Independence: How Hospital Beds Empower Diabetic Patients at Home
Hospital beds designed for home care are vital in helping patients maintain or regain independence, particularly in terms of mobility. Modern homecare hospital beds come with very easy repositioning features reducing frustration with daily use. They enable patients to move more freely, enhancing both their physical comfort and overall well-being.
Here are some ways:
- Simple Repositioning: Patients can adjust their position without assistance, reducing caregiver strain and promoting freedom of movement.
- Smooth Transitions: Elevating the head or legs helps patients sit up, lie down, or stand with less effort.
- Increased Confidence and Stability: Features like side rails or grab bars enhance safety, lowering fall risk and improving stability during movement.
Frequently Asked Questions About Hospital Beds and Homecare for Diabetes
How can a hospital bed assist with diabetic foot care?
Yes, by elevating the feet and providing proper support, a hospital bed can help prevent foot complications related to diabetes. Adjustable bed positions can improve blood circulation to the lower extremities, helping reduce the risk of swelling, pressure ulcers, and other foot-related issues that are common in diabetic patients.
How often should diabetic patients be repositioned in a hospital bed?
Bed-bound patients should be repositioned every two hours. Regular repositioning not only prevents pressure buildup but also improves circulation, which supports healthy skin and reduces the risk of bedsores and other complications associated with prolonged immobility.
Why is frequent repositioning important for diabetic patients in a hospital bed?
Frequent repositioning is widely recommended to prevent pressure sores, tissue damage, and other complications. This practice is especially important for patients confined to bed, as it helps prevent pressure ulcers, or bedsores, which can lead to infections and slow wound healing. Repositioning improves blood flow, supports skin health, and reduces risks tied to immobility.
Can a hospital bed help improve sleep quality for diabetic patients?
Yes, a hospital bed can significantly enhance sleep quality for diabetic patients. Adjustable features allow patients to find comfortable positions that relieve pressure on sensitive areas, reduce pain from diabetic neuropathy, and improve circulation. Elevating the head or legs can also reduce swelling and discomfort, making it easier for diabetic patients to rest. Proper sleep is vital for blood sugar regulation, making a comfortable hospital bed a valuable tool in managing diabetes at home.
What features should I look for in a hospital bed for home care if I have diabetes?
When choosing a hospital bed for diabetes care, look for adjustable height and positioning features, a pressure-relieving mattress, and side rails for added safety. Adjustable positioning helps improve circulation, reduces pressure on the body, and makes it easier for caregivers to assist with tasks. A pressure-relieving mattress minimizes the risk of bedsores, which can be challenging for diabetic patients to heal. Side rails provide support for repositioning, enhancing safety and independence for patients who may need frequent movement assistance.
Conclusion: The Vital Role of Hospital Beds in Supporting Diabetic Homecare
Hospital beds designed for home use are invaluable tools in managing diabetes and its complications, providing essential support that extends beyond basic comfort. For diabetic patients, who often face challenges like reduced mobility, circulation issues, and an increased risk of skin breakdown, a hospital bed at home can make a significant difference. These beds are equipped with features such as adjustable positioning, which not only aids in mobility but also promotes better blood circulation, reducing the likelihood of pressure ulcers and helping with pain relief. This functionality is especially beneficial for patients with diabetic neuropathy, as finding comfortable and supportive positions can be essential for pain management and sleep quality.
Additionally, hospital beds play a critical role in diabetic wound care by enabling caregivers to adjust the bed for easier access during dressing changes and wound inspections, reducing strain on both patients and caregivers. By offering this level of comfort, safety, and accessibility, hospital beds empower diabetic patients to maintain a greater degree of independence at home while reducing the risk of frequent hospital visits due to preventable complications.
With a hospital bed at home, diabetic patients can manage their condition in a familiar and supportive environment. This setting not only promotes better physical health but also positively impacts emotional well-being, as patients can maintain a sense of normalcy and autonomy. By investing in the right hospital bed, diabetic patients and their families can create a homecare setup that supports overall health, enhances quality of life, and provides peace of mind.
Contact Us
At Key Way Medical, we are committed to transforming healthcare through innovation and compassion. Our dedication spans every stage, from research and development to production and distribution, all with the goal of improving lives. By combining cutting-edge technology with compassionate care, we aim to create a world where everyone can live with dignity and independence. If you’d like more information or would like to schedule a live demo of one of our products, please feel free to reach out and contact us today!
References
National Institutes of Health (NIH). (2016). Muscle dysfunction in type 2 diabetes: a major threat to patient’s mobility and independence. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/27393005/
U.S. Department of Health and Human Services. (2024). Health Conditions: Diabetes. Retrieved from: https://odphp.health.gov/myhealthfinder/health-conditions/diabetes
U.S. Centers For Disease Control and Prevention (CDC). (2024). Living with Diabetes. Retrieved from: https://www.cdc.gov/diabetes/living-with/index.html
National Institutes of Health (NIH). (2019). Current situation analysis of diabetic home care patients. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7117632/#:~:text=In%20the%20scope%20of%20the,their%20biochemical%20data%20and%20medications
MedlinePlus. (2023). Turning patients over in bed. Retrieved from: https://medlineplus.gov/ency/patientinstructions/000426.htm
U.S. Centers For Disease Control and Prevention (CDC). (2024). Vision Loss and Diabetes. Retrieved from: https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-vision-loss.html#:~:text=Diabetic%20retinopathy%20(DR)%20is%20the,eyes%2C%20leading%20to%20vision%20loss.
U.S. Centers For Disease Control and Prevention (CDC). (2024). Diabetes – New Beginnings Mini-Lesson: Sleep Health. Retrieved from: https://www.cdc.gov/diabetes/php/toolkits/new-beginnings-sleep-health.html#:~:text=Getting%20enough%20good%20sleep%20helps%3A&text=Keep%20your%20blood%20sugar%20and,physically%20in%20your%20daily%20life.
Better Health Channel. (n.d.) Diabetes – long-term effects. Retrieved from: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-long-term-effects
American Diabetes Association. (2023). Older Adults: Standards of Care in Diabetes—2024. Retrieved from: https://diabetesjournals.org/care/article/47/Supplement_1/S244/153944/13-Older-Adults-Standards-of-Care-in-Diabetes-2024


